Home › State Profiles ›
To understand the strategies that states undertake to expand coverage and initiate broader health reform, it is important to recognize the variability in states’ health coverage distribution, employer-sponsored insurance rates, and public program eligibility levels. The charts below highlight certain aspects of Indiana's coverage landscape.
For more information on specific coverage programs implemented in this state, please click on the ‘Coverage Strategies’ tab.
Overview of Medicaid and SCHIP Coverage[1]
Group | Income Eligibility |
Children[2] | 200% FPL (ages 0-1) 150% FPL (ages 1-19) 250% FPL (SCHIP)[3] |
Pregnant Women | 200% FPL |
Parents (traditional Medicaid) | 25% |
Parents and Childless Adults (HIP)[4] | 200% |
SSI Disabled (non-elderly) | 76% FPL |
Sources of Health Insurance Coverage State Data 2006 – 2007, U.S.[5]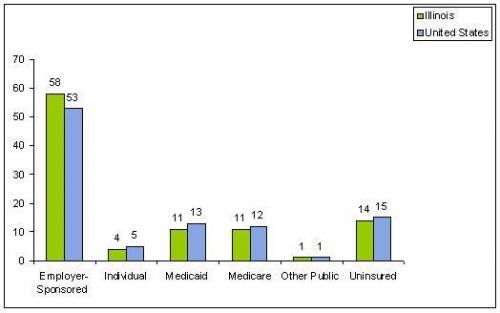
Percentage of Private-Sector Establishments That Offer Health Insurance Based on Firm Size by State, 2006[6] 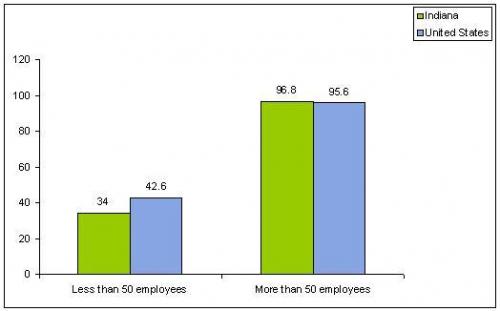
[1]This overview provides a general description of state coverage levels under their Medicaid and SCHIP programs, including coverage through waivers, as of December 2008. Eligibility information was gathered from state web sites, data from state reports, and verified through contacts with CMS and state officials during the fall of 2008. This does not reflect the specific eligibility categories or requirements. This is not intended to be a substitute for eligibility information provided by each state. Individuals interested in applying for these programs should contact the state directly for specific eligibility requirements.
[2]Medicaid eligibility based on children’s family income levels is listed by age group. For states with additional SCHIP eligibility for higher income levels, SCHIP income level eligibility information is presented separately.
[3]As of April 2008, Indiana had a waiver amendment pending approval with CMS to increase the eligibility level to 250% of the PPL for children.
[4]Under the Healthy Indiana Plan section 1115 demonstration, Indiana will provide coverage for custodial parents and caretaker relatives as well as childless adults, otherwise excluded from Medicaid and who have been uninsured for at least 6 months, through 200 percent of the FPL. Under the Medicaid state plan, Indiana provides benefits for parents up to 25 percent of the FPL.
[6]Agency for Healthcare Research and Quality, Center for Financing, Access and Cost Trends. 2006 Medical Expenditure Panel Survey-Insurance Component.



